Survivors SPEAK OUT! Mike Gephart
Survivors SPEAK OUT! Mike Gephart
presented by
Donna O’Donnell Figurski

1. What is your name? (last name optional)
Mike Gephart
2. Where do you live? (city and/or state and/or country)
Oshkosh, Wisconsin, USA
-Email (optional)
3. On what date did you have your brain injury? At what age?
My brain injury happened on March 12, 2014. I was 40 years old.
4. How did your brain injury occur?
I was heading home from work on a 2-lane 55-mph county highway. As I approached an intersection, there was a man waiting in the oncoming lane with his left blinker on. He was struck from behind at 61 mph by an inattentive driver. The man waiting to turn was killed instantly. So less than a second later, I had a 54-mph head-on collision with a dead man (he was pronounced dead at the scene of the accident). 
5. When did you (or someone) first realize you had a problem?
Another person instantly realized I had a major problem.
6. What kind of emergency treatment, if any, did you have?
Twice, on the way to the ER (Emergency Room of a hospital, the EMS (Emergency Medical Service) paramedics got my heart beating. By the time my (now “ex”) wife got there to identify my body, I’d been put on machines. I was in a medically induced coma for nine days, and I was incognizant for 14 more days. After those 23 days, I heard the words “traumatic brain injury,” which described my biggest problem.
7. Were you in a coma? If so, how long?
Yes. I was in a medically induced coma. Of the nine days that I was comatose, two were spent trying to get me out of the coma.
8. Did you do rehab? What kind of rehab (i.e., inpatient or outpatient and occupational and/or physical and/or speech and/or other)? How long were you in rehab?
I was in rehab at the hospital for a week after regaining cognizance. Then I went home and was given physical, speech, and occupational therapies by a home service. Once I could walk with crutches, I had outpatient therapy for another four months.
9. What problems or disabilities, if any, resulted from your brain injury (e.g., balance, perception, personality, etc.)?
I had problems with balance and executive functions. My disability today is basically all about my executive functioning. I had third-party disability insurance through an employer. Because my injuries happened on my way home from work, they got a lawyer to get me on SSDI ASAP (Social Security Disability Insurance; as soon as possible). Because of my executive functioning, “ASAP” meant five years.
10. How has your life changed? Is it better? Is it worse?
I choose not to dwell on all the “bad” things that happened because of my accident. In my 1st or 2nd night of cognizance, crying in my bed alone at 3 am, I had a panic attack about everything that had occurred – and was going to happen. It was at this moment that I heard an internal voice say to me: Mike, bad things happened and will continue to happen far more than anything good.
*Energy you waste fearing Bad is energy you steal from loving Good. (I call that advice “Themandment.” And every one of the 10 commandments that Moses only had to climb a mountain lie safely under the umbrella of Themandment.)
So how has my life changed? I was blessed with clarity and the ability to reinvent my identity in and my understanding of this plane of existence.
11. What do you miss the most from your pre-brain-injury life?
 I miss being in a family unit with my daughters.
I miss being in a family unit with my daughters.
12. What do you enjoy most in your post-brain-injury life?
I’m blessed to know from experience what will happen with my soul when my body dies again.
13. What do you like least about your brain injury?
I don’t like having to acknowledge my brain injury when it reminds me of why I can’t and shouldn’t try being what I was.
14. Has anything helped you to accept your brain injury?
Themandment helps me several times daily.
15. Has your injury affected your home life and relationships and, if so, how?
The relationship with my ex-wife after the accident can’t even be called a relationship.
I came back a new man, and relationships, with what I call “1st Reality Sufferers,” are difficult because of my 2nd perspective.
16. Has your social life been altered or changed and, if so, how?
My social life has changed. I used to be a local rock star with a day job who went where he wanted and felt comfortable. Now, I don’t feel comfortable in many places, I have fewer friends, and I gig far less.
17. Who is your main caregiver? Do you understand what it takes to be a caregiver?
My mother has power of attorney for me, and she is my emergency contact. Early on, my in-laws watched over me while my (now “ex”) wife went back to work.
18. What are your plans? What do you expect/hope to be doing ten years from now?
I don’t plan further than a month yet. My world changed in less than a second. So living in the moment is paramount. 
19. Are you able to provide a helpful hint that may have taken you a long time to learn, but which you wished you had known earlier? If so, please state what it is to potentially help other survivors with your specific kind of brain injury.
Themandment: Energy wasted fearing bad is energy stolen from loving good.
That one passage is a notion I wish I could have had in my 20s. Before my accident, I could spend a day worrying about things that might happen. It hurts to think back to all of the things I didn’t take the time to love and feel blessed to have.
One piece of advice a TBI mentor gave me.
He said: “You didn’t unlearn anything in your accident.
But you need to reinvent a new way to do everything! … with 40 years of experience.”
20. What advice would you offer to other brain-injury survivors? Do you have any other comments that you would like to add?
I suggest three things:
- Themandment
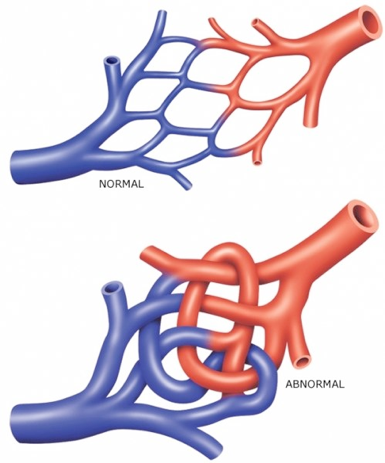
- Reinvent new neuro-pathways.
Relearning how the old ones worked is pointless.
- Unconscious bodily functions!
Focus on things like making it to the toilet on time.
The reason newborns and the elderly wear diapers is because of brand new or deteriorating neuropathways.
Don’t wait for your primary doctor to tell you about it.
*****
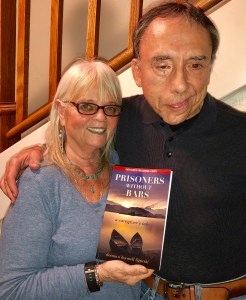
Get Your Copy Now!
Read It! Listen to It! Review It!
Click Links under Book
AUDIO BOOK Listen to it Now!
Stay Safe and Healthy!
Clip Art compliments of Bing.)
(Photos compliments of contributor.)
As I say after each post:
Please leave a comment by clicking the blue words “Leave a Comment” below this post.
Feel free to follow my blog. Click on “Follow” on the upper right sidebar.
If you like my blog, share it intact with your friends. It’s easy! Click the “Share” buttons below.









 10. How has your life changed? Is it better? Is it worse?
10. How has your life changed? Is it better? Is it worse?
 e. ACCEPT THAT LIFE ISN’T FAIR. We need emotions to help us learn. Grow towards the light. Don’t become a weed and strangle those next to you. Treat others as you would want to be treated.
e. ACCEPT THAT LIFE ISN’T FAIR. We need emotions to help us learn. Grow towards the light. Don’t become a weed and strangle those next to you. Treat others as you would want to be treated.







 18. What are your plans? What do you expect/hope to be doing ten years from now?
18. What are your plans? What do you expect/hope to be doing ten years from now?














 Before my accident, I was on a breeder list to get a cavapoo puppy. I was sixth on the list, and a litter was born in May 2021. Some people skipped on this litter of two (the Tom and Jerry litter), so I was able to have my choice. I chose Tom and renamed him Brew. He has been my saving grace after my brain injury. He’s my best friend and constant companion. I don’t know what I’d do without him.
Before my accident, I was on a breeder list to get a cavapoo puppy. I was sixth on the list, and a litter was born in May 2021. Some people skipped on this litter of two (the Tom and Jerry litter), so I was able to have my choice. I chose Tom and renamed him Brew. He has been my saving grace after my brain injury. He’s my best friend and constant companion. I don’t know what I’d do without him.


 18. What are your plans? What do you expect/hope to be doing ten years from now?
18. What are your plans? What do you expect/hope to be doing ten years from now? 20. What advice would you offer to other brain-injury survivors? Do you have any other comments that you would like to add?
20. What advice would you offer to other brain-injury survivors? Do you have any other comments that you would like to add?

Recent Comments