Survivors SPEAK OUT! . . . . . David Figurski . . . . . . . . . . . . . . . 20-Year Post-Injury Anniversary
Survivors SPEAK OUT! David Figurski
20-Year Post-Injury Anniversary
presented by
Donna O’Donnell Figurski
Note:
On April 8, 2014, Donna published my Survivor SPEAK OUT! interview to begin her series of interviews about the experiences and thoughts of survivors and caregivers. Since then, Donna has published over 130 written interviews in which people answer Donna’s twenty survivor- or caregiver-specific questions to let the readers know their stories, tell of their lives, and give first-hand, and often hard-earned, advice for other survivors and caregivers.
In my original interview, I kept my answers short so others wouldn’t be intimidated. I didn’t need to. Other interviewees were not reluctant at all to discuss at length many of the aspects of their brain injuries. In this interview on the 20th anniversary of my TBI (traumatic brain injury), I hope to give you a more detailed look at my past and present life.

1. What is your name? (last name optional)
David Figurski
2. Where do you live? (city and/or state and/or country) Email (optional)

Surprise, Arizona, USA dhfdmf@aol.com
3. On what date did you have your brain injury? At what age?
January 13, 2005 At age 57
4. How did your brain injury occur?
Each morning before showering, I would do Tai Chi warmup exercises and calisthenics. One day, my brain hemorrhaged on my 13th chin-up.
5. When did you (or someone) first realize you had a problem?
I felt something happen in my head, but I didn’t have any pain, so I wasn’t concerned. I stopped exercising because I was seeing double. When my double-vision didn’t clear after a minute or so, I walked down the hall to where my wife (Donna) was getting ready for her job of teaching first-graders. I was exceptionally lucky that day – luck that gave me twenty years more (so far) of life. Normally, I got up at 4:00 am and left for my lab at Columbia University in New York City by 5:30 am. But I was planning to work at home that day to prepare a talk, so I got up later and overlapped Donna’s morning schedule. It turned out to be crucial because Donna saved my life. By the time I got to her, I was in crisis. She immediately saw that my right eye was filled with blood. Not long after, I felt something else happening in my head, and I began experiencing extreme pain. Donna dialed 9-1-1 to get emergency help. I became unintelligible because I was slurring my words. When the paramedics put an oxygen mask on me, the pain subsided, but I slipped into a coma, which lasted nearly three weeks.
6. What kind of emergency treatment, if any, did you have?
The paramedics took me to the Emergency Room of a nearby hospital where Donna made her first life-or-death decision – that I have immediate surgery instead of a CAT (computerized tomography) scan to see if the pressure from the brain-bleed had decreased. It’s clear now that the time that would been taken to do a CAT scan would have decreased my chance of survival by several hundred-fold.

But Donna’s nightmare was only beginning. Over the next two weeks, she had to give permission for two more surgeries on my brain. My chance of survival continued to be low.
After the first surgery, I was carefully transferred by ambulance to Columbia-Presbyterian Hospital in New York City. There, the neurosurgeon discovered an aneurysm that had to be removed. That was the second surgery. I survived … but the neurosurgeon had more bad news for Donna. She had to give permission for another dangerous surgery – to remove an AVM (arteriovenous malformation), a tangle of arteries and veins that can be a “time-bomb.” Miraculously, I survived that surgery too.
(The neurosurgeon at the local hospital for the first surgery was highly skilled, but he gets an F-grade for his manner. His first words after introducing himself to Donna were that I “would make a great organ-donor”!)
7. Were you in a coma? If so, how long?
Yes. I was in a coma for nearly three weeks.
8. Did you do rehab? What kind of rehab (i.e., inpatient or outpatient and occupational and/or physical and/or speech and/or other)? How long were you in rehab?
Yes. A couple of weeks after my surgeries at Columbia-Presbyterian, I was transferred to Radburn Rehabilitation Hospital, which specializes in helping patients with brain injuries. There I had inpatient therapies (physical, occupational, and speech) three days a week for three hours per day. I was discharged from Radburn after about two months, but I continued with outpatient therapies – first at Radburn for three months, and then for two of months at Dominican Hospital in Santa Cruz, California, where our son lives, and then back at Radburn for about a year.
A year after my brain-hemorrhage, I went back to my lab at Columbia University as a volunteer to direct my research group. After I stopped going to Radburn for outpatient therapies (about eighteen months after my brain-hemorrhage), I returned to Columbia University as full-time faculty member. I had a standing appointment for two hours each week with a physical therapist, who worked with me in my office until I retired at the end of August 2013.
9. What problems or disabilities, if any, resulted from your brain injury (e.g., balance, perception, personality, etc.)?
Fortunately, my hemorrhage was at the back of the brain, so no cognitive, memory, or major personality changes resulted from my TBI. I gave lectures, wrote and was awarded a multi-year research grant from the National Institutes of Health, mentored Ph.D. students and postdoctoral scientists, and wrote and published scientific papers. In short, I had my scientific life back – which was really important to me.
But because my cerebellum and brain-stem were primarily affected, I do have several physical disabilities.
I have double-vision from a defective nerve-muscle connection in my right eye. The right side of my face droops from being paralyzed. (The loss of my ability to smile caused me to lose an important part of my self.) My swallow has been affected. It is difficult to eat some foods, and I am always in danger of aspirating. Because the right side of my tongue is paralyzed, it’s difficult to make some sounds and pronounce certain words. (For that reason, I talk less and use fewer words. I have to be careful not to sound curt or rude.) I talk more slowly, and my voice has changed because my vocal cords were affected. (My slower speech allows me to substitute a word mid-sentence to one I can more easily pronounce.) My right arm is ataxic. I can use my left arm and hand for most things, but they are not as good as they once were. (For example, it’s difficult to use my left arm to raise a glass to my mouth, and it’s impossible to do so without shaking.) My right leg is weaker than it was, and my right ankle does not automatically flex the way it should. (I have to consciously focus on my ankle for it to bend properly.) At night, I get up to go to the bathroom about every 90 minutes because I have frequent urinary urges. (Thankfully, this is not a problem during the day.) The cerebellum, which is located at the back of the brain and controls balance, was severely damaged by my hemorrhage. Consequently, my balance is really poor. Donna and I hold each other whenever I walk outside or in a strange environment, like a restaurant. In the house, where the floors are even, I can walk short distances. I use a rollator (4-wheeled walker) for longer walks in the house and an electric scooter for airports and long distances outside.

I feel extremely fortunate that all my disabilities are physical. Of course, my life is now very limited, but I can still read, write, and communicate by using my computer – with my left hand.
10. How has your life changed? Is it better? Is it worse?
Early on, I stopped thinking about what I could no longer do. Instead, I emphasized what I could still do. I then became totally comfortable with my life, and, as a result, my life now is better than it was in many ways. Of course, I would say it’s worse if I continued to grieve what I lost, but I consider that part of my life as gone, like my youth. So I don’t think about what I lost, except to be thankful that I had the chances to do what I did.
11. What do you miss the most from your pre-brain-injury life?

I do miss a couple of things from my pre-TBI life. I miss leaving the house on my own. I miss just doing what I wanted to do without having to carefully plan. I miss Donna’s and my dinner conversations. (Because my damaged cerebellum caused a loss of coordination between my tongue and my teeth, I have to pay close attention to chewing. So Donna and I don’t speak when I’m eating.) I was racing cars, so I desperately miss driving. While I have a device that scans a page and reads it to me, I miss having normal vision and reading books.
12. What do you enjoy most in your post-brain-injury life?
It’s hard to imagine, but my TBI caused me to improve in some areas. Things are much slower (because of my disabilities), so I can’t do as much as I once did. Because I’m slower, I’ve learned to be more efficient and more organized with the time I am able to work. Because I spend nearly all of my time at home, I have more time to be a part of Donna’s life. I have also bonded more closely with and have enjoyed more our dog, a Maltese-Poodle. Koda is a 2-year-old male rescue.

13. What do you like least about your brain injury?
I intensely dislike my loss of balance. It’s an issue that’s a burden not only for me, but also for Donna, who helps me walk whenever we go anywhere.
14. Has anything helped you to accept your brain injury?
I’ve been greatly helped by the positivity of most doctors; the nurses; the therapists; the staff; the Columbia faculty, students, and postdoctoral scientists; and many of the people I’ve come in contact with. But, by far, the greatest help has come from my wife, Donna – the most positive person I know. She cheers every gain – no matter how small. She constantly looks out for me, for example, choosing the easiest path in a restaurant, finding and researching an electric scooter, and bringing home several samples of items so I can choose.
15. Has your injury affected your home life and relationships and, if so, how?
My home life has indeed been affected. I no longer do repairs, so Donna does them. I can’t lift heavy objects, so Donna does what she can and gets help if she needs to. Donna and I do collaborate on some projects. We once had to assemble a piece of furniture. The assembly was complicated, so I laid everything out and understood the directions. I would tell Donna what tool to use and what to do. She was great – she did everything perfectly! Now we have a useful and beautiful cabinet. I used to do everything financial. Now Donna does. She pays the bills, gets everything ready for the tax preparer, and successfully negotiated the deal for our car. I am home a lot more, so we have more time to talk. Among our many conversations are talks about what she and I are feeling in our new life that resulted from my brain injury.
16. Has your social life been altered or changed and, if so, how?
Donna and I weren’t overly social. We continue to socialize in small groups of family and close friends. In the past, our focus was on our two children – and on each other at our weekly “date nights.” Now, we not only focus on our children, but also on their spouses and our grandchildren. Nothing much changed after my TBI, except that I’m always at home and we don’t go out to eat as much anymore.
17. Who is your main caregiver? Do you understand what it takes to be a caregiver?

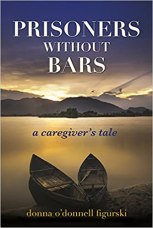
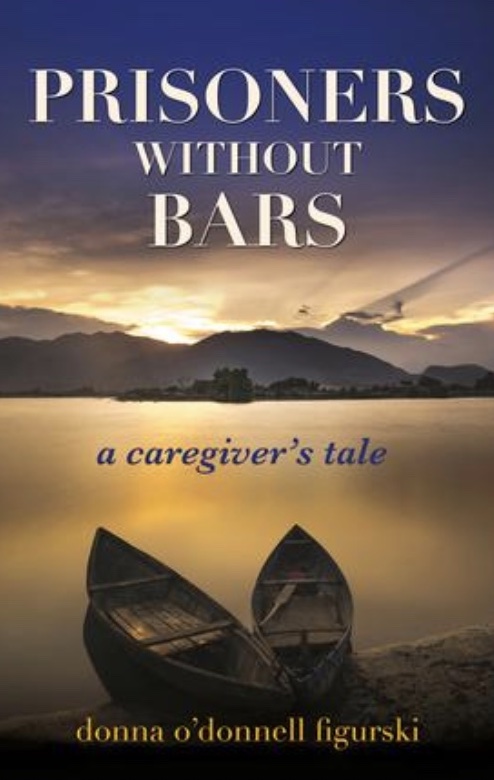
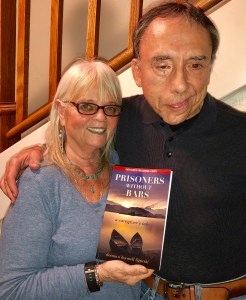
My wife, Donna, has always been my main caregiver. She was with me from the very beginning of my brain injury. Her first acts of caregiving for me were to call 9-1-1 before I slipped into a coma and to advocate for me in the hospitals. Survivors need to realize how heroic their caregivers usually are, how devoted caregivers are to caring for their survivors, how caregivers’ lives have also been severely disrupted – in these cases by brain injury, and how caregivers are often frightened by their survivors’ brain injuries and shocked by the changes to their survivors’ lives. Donna is always using her experiences and knowledge to help other caregivers with what is often an overwhelming responsibility. Donna has published an award-winning memoir (Prisoners Without Bars: A Caregiver’s Tale), which began as daily updates for family and friends around the country. In her updates, she discussed my progress or lack of progress for the day. Later, Donna wrote down what happened in a series of essays to have a record for me. About a year after my hospitalization, she began to read her essays to me. I was shocked by her horrific experience and convinced her to write a book. She did, and a publisher (WriteLife) was interested in her caregiver’s perspective on brain injury. (You can listen to the book trailer below.)
18. What are your plans? What do you expect/hope to be doing ten years from now
In ten years, I expect to continue to focus on the lives of family and friends, continue to learn about and explain science to the public, continue to discuss brain injury with other survivors and with caregivers, continue to help the public understand brain injury, and continue to make Donna’s life as easy as possible.
19. Are you able to provide a helpful hint that may have taken you a long time to learn, but which you wished you had known earlier? If so, please state what it is to potentially help other survivors with your specific kind of brain injury.
Years after my TBI, I gained a perspective that helped me. It’s typical to blame your disability when it takes far longer to accomplish something than you think it should or when you can’t do something you think you should. What helps me is to realize the body is doing the best it can. This minor change of attitude has ended much of my frustration of feeling inadequate. So go easy on yourself.

20. What advice would you offer to other brain-injury survivors? Do you have any other comments that you would like to add?
I can’t emphasize enough the importance of surrounding yourself with positive people. Such people have had a crucial and beneficial effect on my self-esteem. For example, Donna has not only been my caregiver, but she is also my cheerleader. I had an excellent neurologist for years, but then we moved across the country. I found a new neurologist, but Donna and I didn’t feel any positivity from him, so we never returned. Likewise, if a doctor or therapist tells you you can’t do something, and it’s only his or her opinion and is not based experience or data, you may want to find someone else. It’s important for you too to have a positive attitude. At the very least, consider that you survived! Your positive attitude will affect others, especially your caregiver, who is often overwhelmed and who will not be further burdened by your feeling sorry for yourself.
********************************************************************************************************
ADDENDUM reprinted from InTech Open (2013)

Columbia University United States of America
*********************************************************************************************************
Read It! Listen to It! Review It!
Click Links under Book
Stay Safe and Healthy!
Clip Art compliments of Bing.)
(Photos compliments of contributor.)
As I say after each post:
Please leave a comment by clicking the blue words “Leave a Comment” below this post.
Feel free to follow my blog. Click on “Follow” on the upper right sidebar.
If you like my blog, share it intact with your friends. It’s easy! Click the “Share” buttons below















 10. How has your life changed? Is it better? Is it worse?
10. How has your life changed? Is it better? Is it worse?
 e. ACCEPT THAT LIFE ISN’T FAIR. We need emotions to help us learn. Grow towards the light. Don’t become a weed and strangle those next to you. Treat others as you would want to be treated.
e. ACCEPT THAT LIFE ISN’T FAIR. We need emotions to help us learn. Grow towards the light. Don’t become a weed and strangle those next to you. Treat others as you would want to be treated.





 18. What are your plans? What do you expect/hope to be doing ten years from now?
18. What are your plans? What do you expect/hope to be doing ten years from now?












 What is your name? (last name optional)
What is your name? (last name optional)

 When Jordan first came home from rehab, she required help with most of her ADLs (Activities of Daily Living). As time has gone on, she has been able to perform most of her ADLs on her own. She has short-term memory loss, so my role is helping to make sure that she remembers things and stays safe.
When Jordan first came home from rehab, she required help with most of her ADLs (Activities of Daily Living). As time has gone on, she has been able to perform most of her ADLs on her own. She has short-term memory loss, so my role is helping to make sure that she remembers things and stays safe.







Recent Comments