Long COVID . . . . . . . . . . . . . . Serious Long-term Effect of Some COVID-19 Infections
Long COVID – a Serious Long-term Effect of Some COVID-19 Infections
by
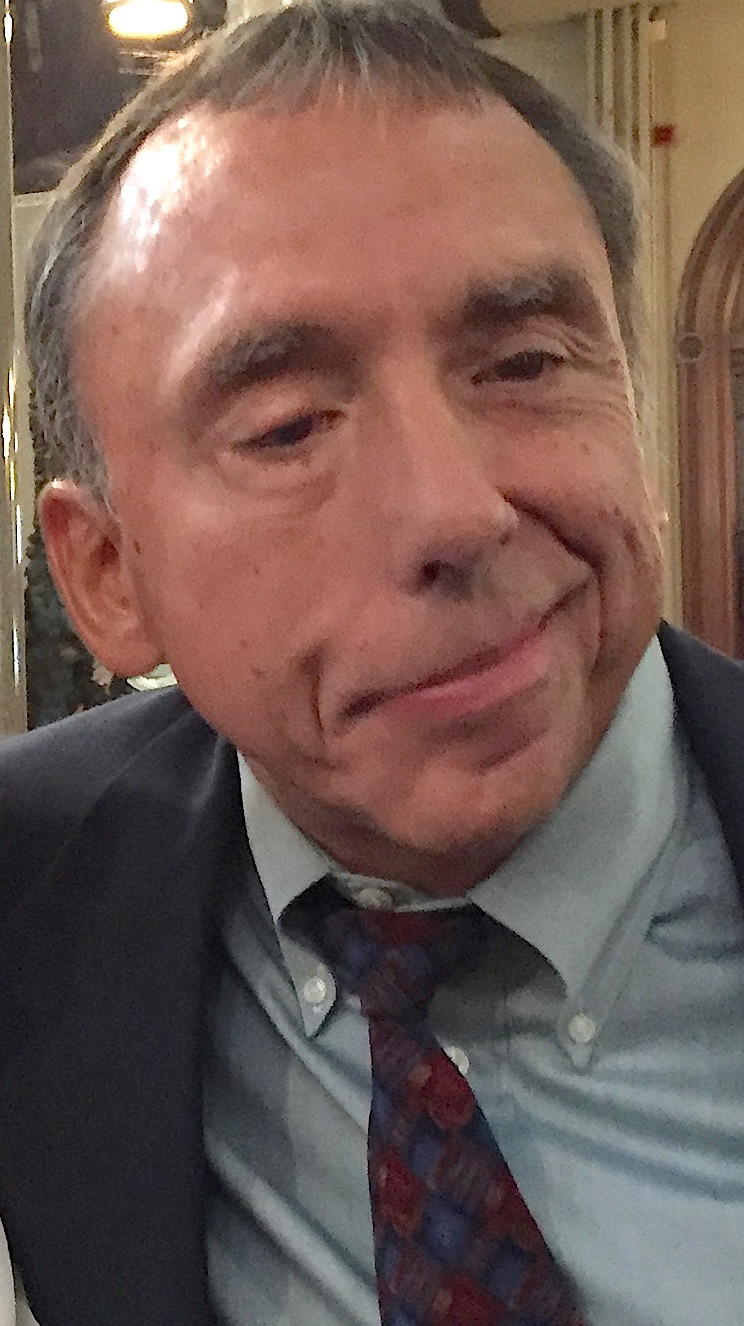
Columbia University Professor Emeritus, Dr. David Figurski
presented by
Donna O’Donnell Figurski
(Disclaimer: The World Health Organization <WHO> has officially named the new coronavirus as SARS-CoV-2 <severe acute respiratory syndrome coronavirus #2> and the disease it causes as COVID-19 <coronavirus infectious disease of 2019>. Because the majority of people, including most of the press, commonly refer to the virus as “COVID-19” or “COVID,” to avoid confusion, I use “COVID-19” as the name of the virus.)

David H. Figurski, Ph.D & Survivor of Brain Injury
Finally – the news I’ve been waiting for!
Bottom line: The news is good … if you’re vaccinated.
Dr. Daniel Griffin, a Columbia University infectious disease physician, has said that long COVID is a public health crisis. Several million people worldwide are living with the mysterious, often disabling, ailments of long COVID.
What is long COVID?
Everybody knows about the acute phase of COVID-19 infection. Some infections are serious and require hospitalization – and maybe intensive care. However, infected people and even the survivors of hospitalization seem to fully recover. They feel fine and test negative for the virus.
But weeks or months later, people who appear to have recovered from a COVID-19 infection may experience any one or several symptoms, which include fatigue, severe headaches, brain fog, anxiety, depression, muscle pain, cough, fever, cognitive impairment, joint pain, chest pain, shortness of breath, vertigo or loss of balance, memory issues, rash, heart palpitations, and sleep issues.
What’s worse – the symptoms can persist. No one knows when the symptoms will end. Some long COVID patients worry that their symptoms will be lifelong. Society needs to be ready for many more disabled people.
Scientists and doctors don’t know the cause.
Particularly worrisome is the fact that even asymptomatic and mild infections can lead to long COVID. Since vaccination still permits asymptomatic and mild infections but prevents the severe infections that require hospitalization, I have been concerned that long COVID can still occur with vaccination. Now it’s clear that vaccination prevents long COVID too.
Because long COVID occurs weeks or months after a COVID-19 infection, it took a while for the data on vaccination and long COVID to come out.
 A recent paper submitted by an Israeli group showed there is a significant reduction (an appropriately conservative conclusion for data that showed 0 cases of long COVID) if a person was vaccinated before getting infected. In contrast, with no vaccination, about half of hospitalized COVID-19 patients will get long COVID. Vaccination after getting COVID-19 helps: Vaccination within 30 days of COVID-19 infection helps reduce the incidence of long COVID significantly. Getting vaccinated 30-60 days after COVID-19 infection helped, but not as much as within 30 days. Getting vaccinated after 90 days post COVID-19 infection does not help.
A recent paper submitted by an Israeli group showed there is a significant reduction (an appropriately conservative conclusion for data that showed 0 cases of long COVID) if a person was vaccinated before getting infected. In contrast, with no vaccination, about half of hospitalized COVID-19 patients will get long COVID. Vaccination after getting COVID-19 helps: Vaccination within 30 days of COVID-19 infection helps reduce the incidence of long COVID significantly. Getting vaccinated 30-60 days after COVID-19 infection helped, but not as much as within 30 days. Getting vaccinated after 90 days post COVID-19 infection does not help.
You can listen to Dr. Griffin talk about long COVID in two short segments – minutes 38:25-41:30 and 47:25-50:15 – of his clinical update in the video podcast (TWiV #856 – This Week in Virology by Columbia virologist Dr. Racaniello.
Get Your Copy Now!
Read It! Review It!
Click Links under Book

PAPERBACK Read Now! eBOOK Read Now! AUDIO BOOK Listen Now!
Stay Safe and Healthy!
Clip Art compliments of Bing.com.
(Photos compliments of contributor.)
As I say after each post
Please leave a comment by clicking the blue words “Leave a Comment” below this post.
Feel free to follow my blog. Click on “Follow” on the upper right sidebar.
If you like my blog, share it intact with your friends. It’s easy! Click the “Share” buttons below.


 Yes. In the past, if anyone called up to do something or to go somewhere, I could easily say “Yes.” It was hard to adjust to a life where I could not. Also, I try to do everything myself, but it is a bit hard whenever people try to help when I really don’t need it.
Yes. In the past, if anyone called up to do something or to go somewhere, I could easily say “Yes.” It was hard to adjust to a life where I could not. Also, I try to do everything myself, but it is a bit hard whenever people try to help when I really don’t need it. 20. What advice would you offer to other brain-injury survivors? Do you have any other comments that you would like to add?
20. What advice would you offer to other brain-injury survivors? Do you have any other comments that you would like to add?
 Columbia virologist Dr. Vincent Racaniello discusses the “mildness” of the omicron variant with Dr. Daniel Griffin, a New York physician in Columbia’ s Department of Infectious Diseases.
Columbia virologist Dr. Vincent Racaniello discusses the “mildness” of the omicron variant with Dr. Daniel Griffin, a New York physician in Columbia’ s Department of Infectious Diseases. 


Recent Comments